Primary intestinal diffuse large B-cell lymphoma (DLBCL)
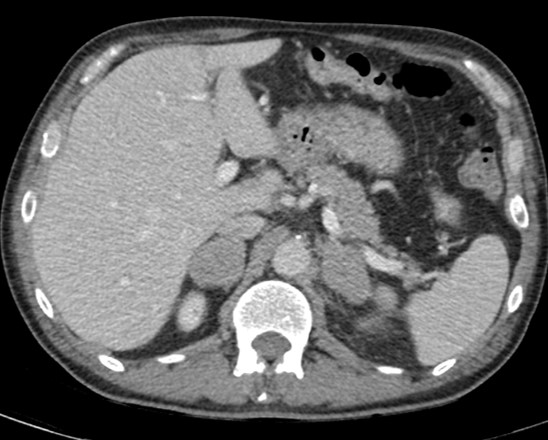
Fig. 1a
Fig. 1b
Fig. 1:
Contrast-enhanced CT (a-c) performed in a 63-year-old male patient that presented with vomiting and fever and referring diffuse abdominal pain and unexplained weight loss in the months prior to ER visit. Axial CECT images reveal jejunal loops parietal thickening in epigastrium (arrow, a) and umbilical region (arrow, b).
Fig. 1c
Fig. 1:
Furthermore, CECT axial image shows bilateral adrenal solid masses (arrows, c) suspicious for metastasis.
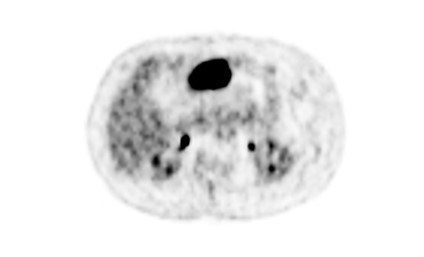
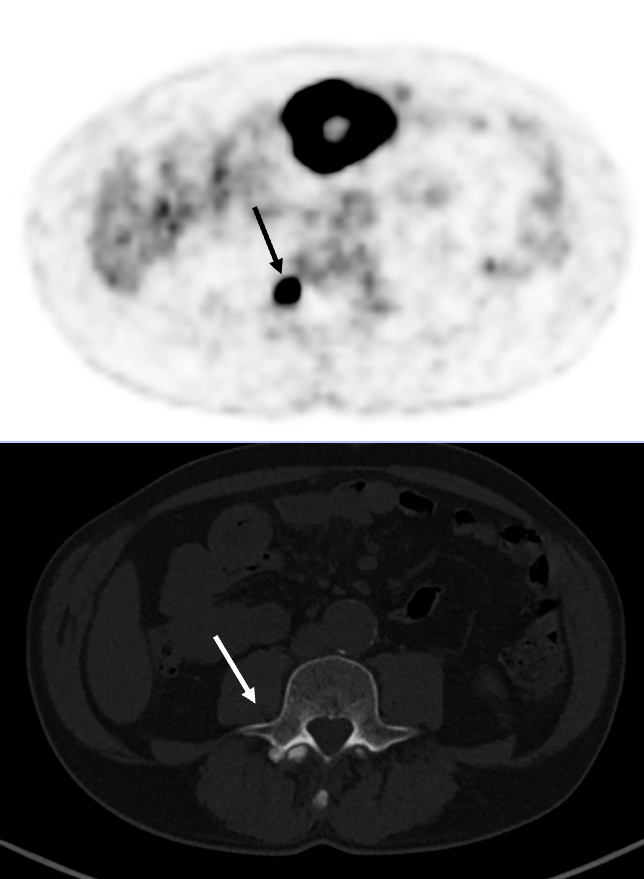
Fig. 2a
Fig. 2b
Fig. 2:
18F-FDG-PET (a-c) was performed 3 weeks later. Axial images confirm extensive metabolically active disease at the level of the small intestine bowel loops thickening previously seen on CECT in the epigastrium (arrow, a) and umbilical region (arrow, b). At both bowel sites, FDG uptake is markedly increased in comparison to the liver, indicating a Deauville criteria score (DS) of 5.
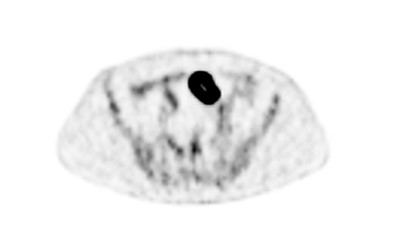
Fig. 2c
Fig. 2:
8F-FDG-PET also confirmed intense uptake at the level of both adrenal glands masses, compared to liver metabolic activity (DS=5), confirming the suspect of metastases
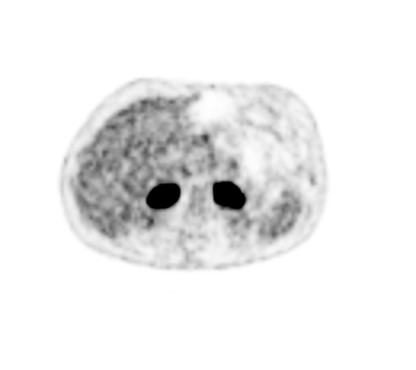
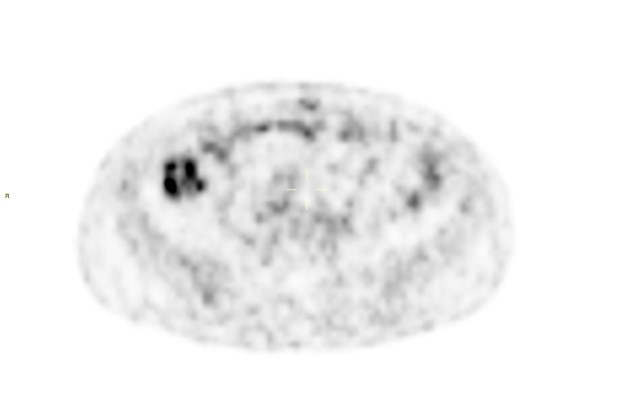
Fig. 3a
Fig. 3b
Fig. 3
Comparison of PET (first row) and CECT (second row). Metabolically active bone disease not readily visible in CECT at the level of L4 (arrow, a) and D3 (arrow, b).
Clinical course and diagnosis
Following CT and PET findings, the patient underwent anterograde enteroscopy and biopsy of the diseased intestinal loop that confirmed the diagnosis of intestinal B-cell lymphoma (CD20+ CD5- CD10-).
Combined immuno-chemotherapy was started (6 cycles R-CHOP).
One month later, during the 2nd cycle of chemotherapy, the patient presented to the ER with diffuse abdominal pain and distension. CECT evidenced pneumoperitoneum related to the perforation of the diseased bowel loop. Surgical resection was performed.
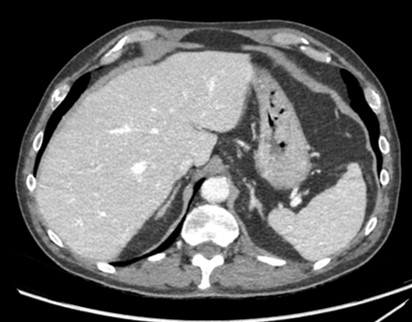
Fig. 4a
Fig. 4
Interim 18F-FDG-PET performed after 3 cycles of therapy shows complete metabolic resolution of intestinal, adrenal and skeletal disease (not shown). However, there was slight metabolic activity (SUV peak 4,5) at the level of the ascending colon (arrow), likely related to the recent surgical procedure rather than to active disease. Therefore, the corresponding assigned Deauville criteria score was DS X.
Fig. 5a
Fig. 5b
Fig. 5
CECT was performed after completing the 6th cycle of chemotherapy. On axial images (a and b) intestinal loops present regular caliber without any signs of occlusion; surgical resection margins are smooth. Moreover, complete regression of adrenal enlargement (arrows, b) is evident and both glands show a regular thin and smooth outline.
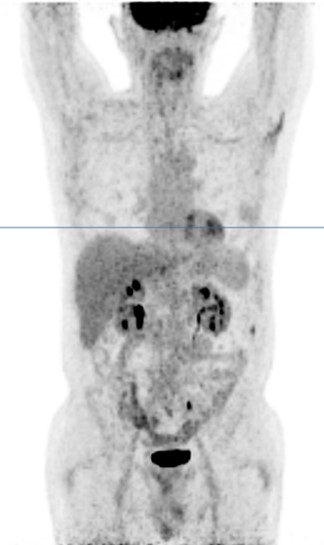
Fig. 6a
Fig. 6
18F-FDG-PET-CT performed a the end of treatment. No FDG-avid lesions distinctive for active lymphoma or recurrent disease in previously affected bowel loops and at the adrenal glands are evident, confirming complete response following immuno-chemotherapy.
Summary:
- Diffuse large B-cell lymphoma (DLBCL) is the most common histological subtype of Non-Hodgkin’s lymphoma (NHL) accounting for approximately 32%.
- It typically presents as a rapidly enlarging mass at a nodal (N-DLBCL) or extranodal site (EN-DLBCL) and can arise virtually anywhere in the body.
- Primary gastrointestinal diffuse large B-cell lymphoma (PGI-DLBCL) is the most common of all extranodal DLBCL and usually presents in the stomach, the small intestine and/or colon.
- PGI-DLBCL with bilateral adrenal involvement is a very rare occurrence and there are only few cases reported in literature.
- DLBCL is highly FDG-avid and therefore FDG-PET/CT constitutes the standard for staging the disease (Lugano criteria) and in the evaluation of response to therapy (Deauville criteria, 5 point scale), both for nodal diseases and cases with extranodal involvement.
- The new Lugano classification states that bone marrow biopsy can be obviated in case FDG-PET/CT is clearly positive for bone marrow involvement but may still be necessary in other cases.
- According to some Authors, contrast-enhanced CT examination should still be included at initial staging for optimal anatomic assessment and accurate measurements.
- DLBCL is a highly aggressive tumor but curable for most patients with the appropriate treatment. The standard first-line therapy consists of combined immuno-chemotherapy with R-CHOP regimen and CNS prophylaxis with methotrexate.
- Common gastrointestinal complications that can occur during or after therapy are perforation, obstruction and gastrointestinal bleeding.
This Case was kindly provided by:
Dr. Constanze Husen (resident)
School of Medicine, University of Milano-Bicocca, Milan
Department of Radiology, Papa Giovanni XXIII Hospital, Bergamo – Italy
Dr. Bonaffini Pietro Andrea (staff)
School of Medicine, University of Milano-Bicocca, Milan
Department of Radiology, Papa Giovanni XXIII Hospital, Bergamo – Italy
Dr. Valle Clarissa (staff)
School of Medicine, University of Milano-Bicocca, Milan
Department of Radiology, Papa Giovanni XXIII Hospital, Bergamo – Italy
Prof. Sironi Sandro (chief)
School of Medicine, University of Milano-Bicocca, Milan
Department of Radiology, Papa Giovanni XXIII Hospital, Bergamo – Italy